The Bay Area Hearing Voices Board wrote the following letter in response to a Huffington Press post criticizing the HVN by Canadian parent advocate Susan Inman. Multiple organizations and individuals have signed on, including Hearing Voices Network NYC. If you want to sign it too, contact the Bay Area HVN group here .
.
……………………………………………………….
Dear Editors,
We write to express our concern and misgivings about Susan Inman’s recent post (“What You’re Not Hearing About the Hearing Voices Movement”). Ms. Inman has profoundly mischaracterized hearing voices networks (HVNs) and also demonstrates a troubling lack of understanding of the empirical literature on psychosis, optimal psychosocial intervention and recovery.
We–the Bay Area Hearing Voices Network (BAHVN)–are a regional HVN that includes peers, family members, clinicians, and researchers. Many of the peers who attend our groups (and the loved ones of affiliated family members) take–and benefit from–antipsychotic medications. Many of us have also struggled (personally or within our families) with very “severe” and disabling forms of psychosis and are no strangers to the enormous challenges involved. Instead it is precisely in response to the enormity of these challenges that we undertake the work we do. Our goal is not to challenge psychiatry, but rather to create spaces in which dialogue is possible, and in which the personal meaning of psychotic experiences (and their social and cultural contexts) are centered.
There is no sense in which the mission of our group (or any regional or national HVN, to our knowledge) is to discourage medication use; instead we emphatically stress the highly individual nature of voices and psychosis and the importance of both peers and family members exploring what works for them. Medications are only one possible aid in an evidence-based and evidence-informed toolbox that includes peer support, psychosocial rehabilitation, community reintegration and an array of therapies (including mindfulness and compassion-focused therapy for voices; Thomas et al., 2014). An open access special issue of Schizophrenia Bulletin (the leading schizophrenia research journal) published last year, covers many of these issues including a review of psychosocial approaches to auditory hallucinations, a paper on distinct voice sub-types, auditory hallucinations in both with and without a need for care and a peer-reviewed overview of the hearing voices network approach.
Turning to the scientific literature more broadly, Ms. Inman’s post appears largely ignorant of research on voices and psychosis over the past two decades. Socioenvironmental causes and contributories are well-documented, including childhood sexual trauma and bereavement (Bebbington et al., 2011; Bentall & Fernyhough, 2008; Kirkbride et al., 2014; Matheson et al., 2013; Varese et al., 2012). Leading biomedical researchers have repeatedly underscored that “schizophrenia” is a misleading term implies a false unity of multiple, etiologically distinct, “psychoses” (Keshavan et al., 2013). Voices (or auditory verbal hallucinations) are found at high rates across diagnoses, including major depression, PTSD and DID. Estimates of voice hearing in the healthy (non-clinical) general population range from 5-15% (Beavan et al., 2013). In reviewing Marius Romme’s research, Ms. Inman decontextualizes a body of work that has largely focused on the range of voices (or auditory hallucinations) occurring outside the schizophrenia spectrum and within healthy populations, at present a large and active area of research for many scientists and epidemiologists (see the work of the International Consortium on Hallucination Research).
Clinical researchers and stigma experts have amply demonstrated that “biomedical” explanations of schizophrenia increase (rather than alleviate) stigma, for instance exacerbating the general public’s belief that people with schizophrenia are “dangerous” and decreasing the hope and self-esteem of peers (Angermeyer et al., 2013, 2014; Kvaale et al., 2013ab; Schomerus et al., 2012). A recent study suggests that individuals who endorse a biomedical view of their experiences are also significantly less likely to benefit from cognitive behavioral therapy, currently the front-line evidence-based therapy for psychosis in Canada, the US and the UK (Freeman et al., 2013).
Research attesting to the importance of engaging with and integrating the symptoms and experiences of psychosis with one’s identity and sense of self (“integrating” versus “sealing off”) goes back to the 1970s and has continued up to the present (McGlashan et al., 1975; Thompson et al, 2003; de Jager et al., 2015). Decades of work on factors involved in recovery attest to the importance of peer relationships, sense of belonging, and the active exploration of the impact of one’s symptoms on one’s life (e.g. Sells et al., 2003; Davidson et al., 2008).
Finally, Ms Inman’s use of “evidence based practices” concerns us. The “evidence base” is constantly evolving and new interventions (that do not yet have evidence behind them) are continuously piloted and evaluated. Current treatments fail many. Antipsychotic medications are only partially effective or ineffective for a large percentage of persons diagnosed with schizophrenia (this is not a controversial claim); likewise the long-term impact of evidence-based strategies such as early intervention for psychosis remain inadequate. Ten year follow-up data for the important OPUS trial of early intervention, for example, found no difference between participants and controls provided treatment as usual in employment, education, or marital status after ten years; the vast majority of individuals across groups were unemployed and struggling; Secher et al., 2014). Even “good responders” to medications all too often do not recovery socially–i.e. in the sense of employment or community integration–without psychosocial supports and social intervention (Morgan et al., 2014).
As any scientist would agree–and certainly those of us intimately affected by psychosis–we must continually innovate, test new strategies and interventions and provide hope and support to both peers and family members.
We encourage Ms Inman (and everyone) to join us in respectful dialogue, and to critically and objectively read and engage with lived experience, clinical experience and the research literature.
The Board of the Bay Area Hearing Voices Network
Co-signatories:
Dirk Corstens MD on behalf of the InterVoice Board
Ron Coleman & Karen Taylor, Working to Recovery
Hearing Voices Network–New York City
Chicago Hearing Voices
NAMI Pennsylvania Montgomery County
Dr. Cherise Rosen, Department of Psychiatry, University of Illinois at Chicago
Dr. Sarah Keedy, Department of Psychiatry, University of Chicago
Dr. Neil Thomas, Senior Lecturer in Psychology, Swinburne University & Director,
Voices Clinic at Monash Alfred Psychiatry Research Centre
References
Angermeyer, M. C., Daubmann, A., Wegscheider, K., Mnich, E., & Schomerus, G. (2014). The relationship between biogenetic attributions and desire for social distance from persons with schizophrenia and major depression revisited. Epidemiology and Psychiatric Sciences, 1-7.
Bebbington, P., Jonas, S., Kuipers, E., King, M., Cooper, C., Brugha, T., … & Jenkins, R. (2011). Childhood sexual abuse and psychosis: data from a cross-sectional national psychiatric survey in England. The British Journal of Psychiatry, 199(1), 29-37.
Bentall, R. P., & Fernyhough, C. (2008). Social predictors of psychotic experiences: specificity and psychological mechanisms. Schizophrenia Bulletin, 34(6), 1012-1020.
Corstens, D., Longden, E., McCarthy-Jones, S., Waddingham, R., & Thomas, N. (2014). Emerging perspectives from the Hearing Voices Movement: implications for research and practice. Schizophrenia Bulletin, 40(Suppl 4), S285-S294.
Davidson, L., Schmutte, T., Dinzeo, T., & Andres-Hyman, R. (2008). Remission and recovery in schizophrenia: practitioner and patient perspectives. Schizophrenia Bulletin, 34(1), 5-8.
de Jager, A., Rhodes, P., Beavan, V., Holmes, D., McCabe, K., Thomas, N., … & Hayward, M. (2015). Investigating the Lived Experience of Recovery in People Who Hear Voices. Qualitative Health Research, 1049732315581602.
Freeman, D., Dunn, G., Garety, P., Weinman, J., Kuipers, E., Fowler, D., … & Bebbington, P. (2013). Patients’ beliefs about the causes, persistence and control of psychotic experiences predict take-up of effective cognitive behaviour therapy for psychosis. Psychological Medicine, 43(02), 269-277.
Keshavan, M. S., Clementz, B. A., Pearlson, G. D., Sweeney, J. A., & Tamminga, C. A. (2013). Reimagining psychoses: an agnostic approach to diagnosis. Schizophrenia Research, 146(1), 10-16.
Kirkbride, J. B., Jones, P. B., Ullrich, S., & Coid, J. W. (2012). Social deprivation, inequality, and the neighborhood-level incidence of psychotic syndromes in East London. Schizophrenia Bulletin, sbs151.
Kvaale, E. P., Gottdiener, W. H., & Haslam, N. (2013). Biogenetic explanations and stigma: A meta-analytic review of associations among laypeople. Social Science & Medicine, 96, 95-103.
Kvaale, E. P., Haslam, N., & Gottdiener, W. H. (2013). The ‘side effects’ of medicalization: A meta-analytic review of how biogenetic explanations affect stigma. Clinical Psychology Review, 33(6), 782-794.
Matheson, S. L., Shepherd, A. M., Pinchbeck, R. M., Laurens, K. R., & Carr, V. J. (2013). Childhood adversity in schizophrenia: a systematic meta-analysis. Psychological Medicine, 43(02), 225-238.
McCarthy-Jones, S., Thomas, N., Strauss, C., Dodgson, G., Jones, N., Woods, A., … & Sommer, I. (2014). Better than mermaids and stray dogs? Subtyping auditory verbal hallucinations and its implications for research and practice. Schizophrenia Bulletin., 40(Suppl 4), S275-S284.
McGlashan, T. H., Levy, S. T., & Carpenter, W. T. (1975). Integration and sealing over: clinically distinct recovery styles from schizophrenia. Archives of General Psychiatry, 32(10), 1269-1272.
Morgan, C., Lappin, J., Heslin, M., Donoghue, K., Lomas, B., Reininghaus, U., … & Dazzan, P. (2014). Reappraising the long-term course and outcome of psychotic disorders: the AESOP-10 study. Psychological Medicine, 44(13), 2713-2726.
Schomerus, G., Schwahn, C., Holzinger, A., Corrigan, P. W., Grabe, H. J., Carta, M. G., & Angermeyer, M. C. (2012). Evolution of public attitudes about mental illness: a systematic review and meta‐analysis. Acta Psychiatrica Scandinavica, 125(6), 440-452.
Secher, R. G., Hjorthøj, C. R., Austin, S. F., Thorup, A., Jeppesen, P., Mors, O., & Nordentoft, M. (2014). Ten-year follow-up of the OPUS specialized early intervention trial for patients with a first episode of psychosis. Schizophrenia Bulletin, sbu155.
Sells, D. J., Stayner, D. A., & Davidson, L. (2004). Recovering the self in schizophrenia: An integrative review of qualitative studies. Psychiatric Quarterly, 75(1), 87-97.
Thomas, N., Hayward, M., Peters, E., van der Gaag, M., Bentall, R. P., Jenner, J., … & McCarthy-Jones, S. (2014). Psychological therapies for auditory hallucinations (voices): Current status and key directions for future research. Schizophrenia Bulletin, 40(Suppl), S202-S212.
Thompson, K. N., McGorry, P. D., & Harrigan, S. M. (2003). Recovery style and outcome in first-episode psychosis. Schizophrenia Research, 62(1), 31-36.
Van Os, J., Rutten, B. P., & Poulton, R. (2008). Gene-environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophrenia Bulletin, 34(6), 1066.
Varese, F., Smeets, F., Drukker, M., Lieverse, R., Lataster, T., Viechtbauer, W., … & Bentall, R. P. (2012). Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective-and cross-sectional cohort studies. Schizophrenia Bulletin, 38(4), 661-671.
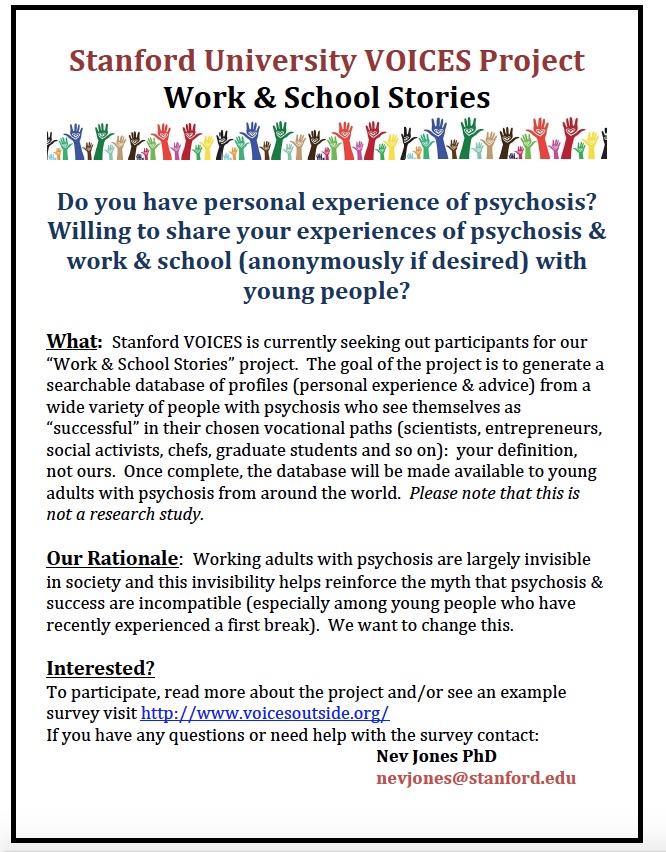
 hat is the Hearing Voices Network up to in the USA, and how is it acting to spread this new model of support?
hat is the Hearing Voices Network up to in the USA, and how is it acting to spread this new model of support?